
Build a scalable remote patient monitoring and virtual care program to reduce ED utilization and readmissions, resulting in reductions in costs for your most at-risk patients.
Leverage AMC Health’s 20 years of experience as a consultative virtual care facilitator, offering enhanced care coordination with Remote Patient Monitoring (RPM) and Tele-Care management (TCM) solutions for patients with chronic conditions, high-risk pregnancies, and complex diseases including cancer and behavioral health.
AMC Health supports and scales chronic condition and post-acute care management programs empowering payers, providers, and patients.
- Personalized Patient Solutions
- Multiple program design options
- Scalable
- Proven and Guaranteed ROI
.png?width=2100&height=1500&name=MicrosoftTeams-image%20(119).png)
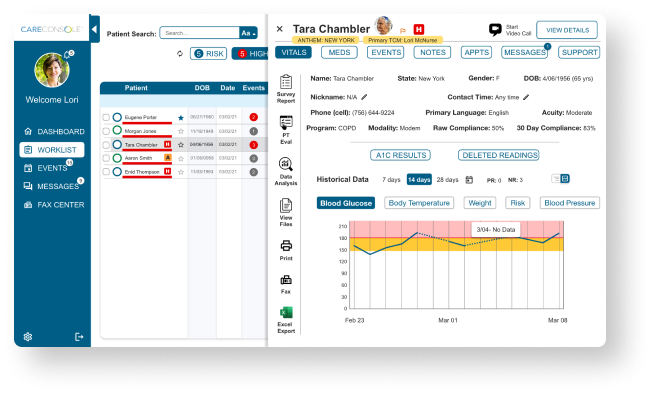
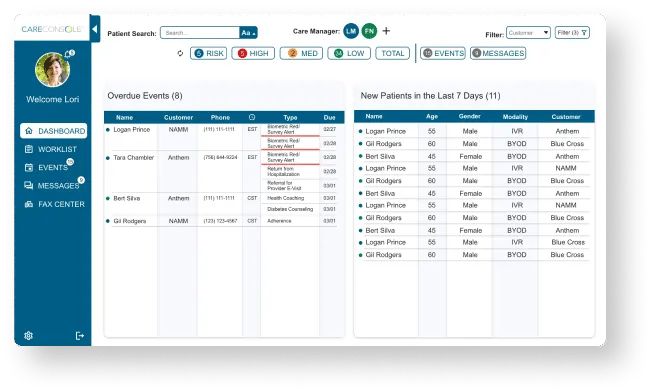
AMC Health’s FDA Class II cleared, clinically proven care management platform manages remote care programs for a wide variety of patient populations across all care settings. Our platform makes your disease management and post-acute-care programs more efficient and effective.
All our devices are wireless for convenience and easy to use on a daily basis regardless of age and location.
Provide better care and better access to care for members and let them take charge of their own health.
Real-time patient data can be accessed easily through our Care Console platform and by your patients through the AMC Healthapp.
Real-time patient data can be accessed easily through our Care Console platform and by your patients through the AMC Healthapp.
Real-time patient data can be accessed easily through our Care Console platform and by your patients through the AMC Healthapp.
Real-time patient data can be accessed easily through our Care Console platform and by your patients through the AMC Healthapp.
AMC Health’s Virtual Care, Telehealth and Remote Patient Monitoring (RPM) Solutions are designed to engage your members, enhance care delivery, support your value-based partners.
All of our devices are wireless for convenience and easy to use on a daily basis regardless of age and location.
Provide better care and better access to care for members and let them take charge of their own health.
Real-time member data and machine learning capabilities identifies rising risk and is accessible through our Care Console platform.
AMC’s strategy for reducing alert fatigue ensures your clinical team is not unnecessarily overwhelmed.
If additional resources are needed, AMC can provide telecare management and full virtual clinical resources, certified in all 50 states.





.jpeg?width=2000&name=AdobeStock_450901146%20(1).jpeg)


